What is Fungal Acne and How Do I Know If I Have It?
Find out if your breakout is not the garden-variety type.

Are those angry red bumps on your skin just your typical acne or are they something else completely? If your skin is always breaking out and nothing you do or use seems to be working, then maybe they aren’t even regular acne at all. You could be suffering from what’s known as fungal acne. And because, for the most part, fungal acne looks like regular acne, they’re often misdiagnosed as such.
What is Fungal Acne?
Fungal acne occurs when the hair follicles on the skin become infected by the fungus Malassezia, which is naturally found on the skin, causing folliculitis that appears as red bumps.
What’s the Difference Between Common Acne and Fungal Acne?
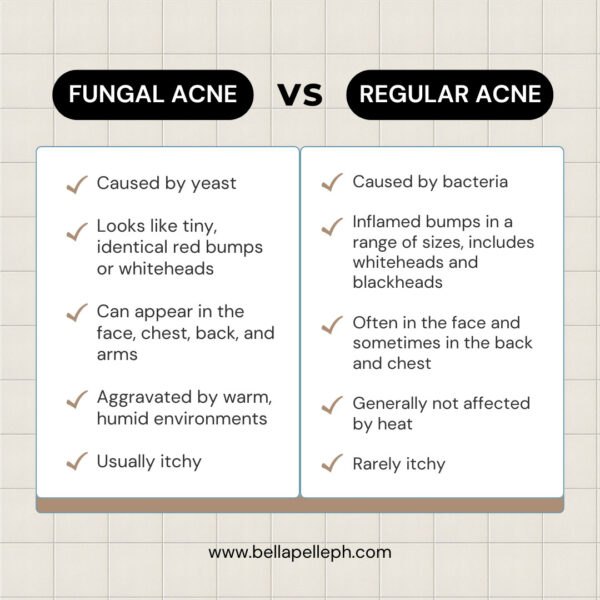
Fungal acne, like the common acne, causes red bumps that can become inflamed and turn into whiteheads. But unlike the common acne or acne vulgaris, which results from hair follicles getting blocked with bacteria, oil, and dead skin, fungal acne is a fungal infection in the hair follicles. “Also called Malassezia folliculitis or Pityrosporum folliculitis, fungal acne is caused by Malassezia furfur, a yeast growing in the hair follicle, causing inflammation,” explains Dr. Maximin Navarro, resident dermatologist at Bella Pelle Skin Solutions and a Philippine Dermatological Society (PDS) fellow.
“Fungal acne can be confirmed by performing KOH smear which will show clusters of hyphae and yeast cells, resembling a ‘spaghetti and meatballs’ pattern,” he adds. “Also, a skin punch biopsy of the skin lesion will show yeast cells on the superficial layer of the skin, the stratum corneum, and can be confirmed by doing Periodic Acid Schiff-Stain (PAS).”
Other clues that it’s fungal acne and not your regular acne? They are more or less uniform in size, appear in clusters, can occur on the arms, chest, and back, and are itchy—which is probably the most telltale sign. What’s more, they don’t respond to your typical acne medications.
What Causes Fungal Acne?
Because fungal acne is caused by fungus or yeast, conditions that promote yeast growth and/or change the skin’s biome can lead to fungal acne. “Predisposing factors such as excessive sweating due extreme hot temperature and [practicing] poor hygiene—such as not changing clothing when soaked with sweat—may promote the growth of yeast in the skin,” says Dr. Navarro. And because yeast thrives in warm and moist environments, fungal acne tends to flare in the summer months.
Antibiotic and steroid/prednisone medications can also be blamed, as well as many antibacterial acne treatments—medications that can eliminate normal skin bacteria and create an optimal environment for yeast to proliferate and fungal acne to flare.
This condition is most likely to be seen in people who sweat a lot or have hyperhidrosis, have a weakened immune system, suffer from other fungal infections, such as seborrheic dermatitis or tinea versicolor, or use a lot of oil-based moisturizers and sunscreens. Add to that practices that can lead to folliculitis, like leaving your skin hot and damp, plucking or waxing hair, frequently touching or rubbing your skin, using a hot tub or whirlpool, or wearing tight clothes, and you have a recipe for fungal acne.
How do you treat fungal acne?
Your regular acne treatments won’t work and might even make things worse. Most dermatologists recommend anti-yeast and antifungal treatments. For mild cases, you can apply topical antifungal cream or lotion daily to affected areas. “Antifungal shampoo or products containing Zinc Pyrithione, Ketoconazole or Miconazole may be used,” says Dr. Navarro. “To apply: Wet the affected areas, apply the product, and leave it on for 10 to 15 minutes before washing.“
Try: Bioderma Nodé DS + Anti Recidive Shampoo, P1,550
The DSactive® patented complex guarantees dual efficacy by targeting the cause— Malassezia yeast. It limits its proliferation and prevents recurrences by minimizing sebum secretion, which causes Malassezia to spread.

Kamedis SEBO Dandruff Shampoo / Scalp Control Dandruff Shampoo, P1,350 – P2,600
Thanks to its unique Triple Action Formula featuring Botaniplex™, zinc pyrithione, and salicylic acid, this zeroes in on the root cause. It provides immediate and effective soothing relief and is safe and gentle for children three years and older, yet potent enough for adults.
This multi-action shampoo is formulated to regulate sebum, delivers keratolytic and kerato-regulating results, and provides in-depth hydration.
Also helpful: Psorolin Medicated Bathing Bar, P450, to exfoliate and soothe skin, preventing fungal buildup.
For more persistent or recurring fungal acne, your doctor might need to prescribe oral antifungal medication and put you on a maintenance treatment. If conditions fail to improve, consult with a board-certified dermatologist to determine the best course of action.
For customized skin and hair care recommendations, you can book a virtual or face-to-face dermatological consultation with Dr. Maximin Navarro, our resident dermatologist, and a Philippine Dermatological Society (PDS) fellow, here. You can also inquire at the Bella Pelle Skin Solutions Center via (+63) 999-887-1944. View the full menu of services and treatments here.
For more beauty and skincare tips, subscribe to our newsletter:
SHOP OTHER PRODUCTS:
 Bella Pelle Tea Tree Bar Soap, P195 |
 Aknicare Gentle Cleansing Gel, P1,990 |
 Biretix Oral, P1,380 |
 Kamedis AC-Clear Face Cleanser, P1,300 |